Poker, one may reasonably argue, is a game of sheer luck; he (or she) who happens upon the most desirable combination of cards will likely win the round of bets. However, as seasoned players know, the art of poker lies in its psychology. The ability of the player to keep an emotionless persona not just when dealt an appealing hand but especially when dealt a bad one—the poker face—is how competitors can trick each other to win in high stakes situations regardless of their cards.
I find at times medical school to be like a big poker game, with its players the medical students. The stakes are plentiful: a “bet” of a couple hundred thousand dollars that a medical degree will be obtained, a desired specialty (though I am in awe how some of us have already chosen or eliminated fields within months of donning the white coat), a coveted residency program, a preferred lifestyle, and more. With our futures on the line, it is thus natural that we all play our cards to the best of our abilities.
In this high stakes, high self-expectations environment of medical school, I have learned that we often wear masks of professionalism and composure in front of our peers, internalizing our fears of underperforming and stresses of daunting course loads. I, like many of my classmates, have walked into the anatomy lab with an air of confidence yet minimal knowledge of what structures I am trying to expose during my dissection; I have sat through a lecture stone-faced while my mind struggles to grasp the content before me; I have chatted with friends days before an exam with a calm demeanor while internally agonizing at how hopelessly behind I am in my studies. Why is there a disconnect between what many of us feel and show during this transition to medical school?
I attribute much of this professional masking to the social comparison theory(1). The theory, formulated in the 1950’s by acclaimed social psychologist Leon Festinger, proposes that humans are always striving to evaluate their own abilities. In situations where an objective evaluation mechanism does not exist, humans will compare themselves to others in order to satisfy that desire for self-evaluation.
Grades are an objective comparative measure that fuels competition at the initiation of medical school, but there are also other objective and (more numerous) non-objective factors that we often use as a means of self-evaluation—demeanors of our colleagues (which provide a perceived level of intelligence), abilities to ask and answer complex questions during class, involvement in other activities outside of studying, and prior knowledge that is brought to the table during relevant clinical scenarios, among others. When we compare ourselves to our classmates using subjective factors, factors that are likely poor indicators of future success as students and physicians, we are inherently creating an environment in which we are constantly looking at others to gauge our own self-worth. Unfortunately, when we find that there is always someone who is better in some aspect of those subjective measures, we don poker faces around peers to hide our own supposed bad hand of cards.
In computer science and statistics, we know that when the data we input into an algorithm is incorrect or improperly sampled, the results are themselves useless—garbage in, garbage out. Similarly, when the factors we use to compare one another are fabricated out of our own personal beliefs about what a successful medical student is like, the comparisons with which we conclude are consequently fabricated themselves. The point of the matter is that when we compare ourselves to our classmates through subjective and vague means, we are setting the stage for consistent stress in an environment that should focus on passionate discovery and lifelong learning.
I argue that there is no truly objective measure of medical student success—we all have our own stories to cultivate—and thus measuring one’s own progress through interpersonal comparisons will inevitably lead to dissatisfaction and stress. As numerous studies in medical education have found, medical student distress has dangerous implications on the mental health of future physicians(2).
So the question remains: How do medical students avoid getting trapped in interpersonal comparisons within a career of continuous competition? I provide some key solutions that medical students and faculty members can work together to achieve:
Festinger’s social comparison theory, in addition to shedding light on the basics of comparative self-evaluation, also suggests that individuals are less likely to compare themselves to people who are different from them. While on the surface it may seem that medical school classes are relatively homogeneous—overall strong academic profiles, clinical experiences, and volunteer activities—each student already has or can participate in new unique experiences that highlight his or her strengths. In establishing a sense of individuality, medical students can avoid comparing themselves to their peers while discovering their passions for the field.
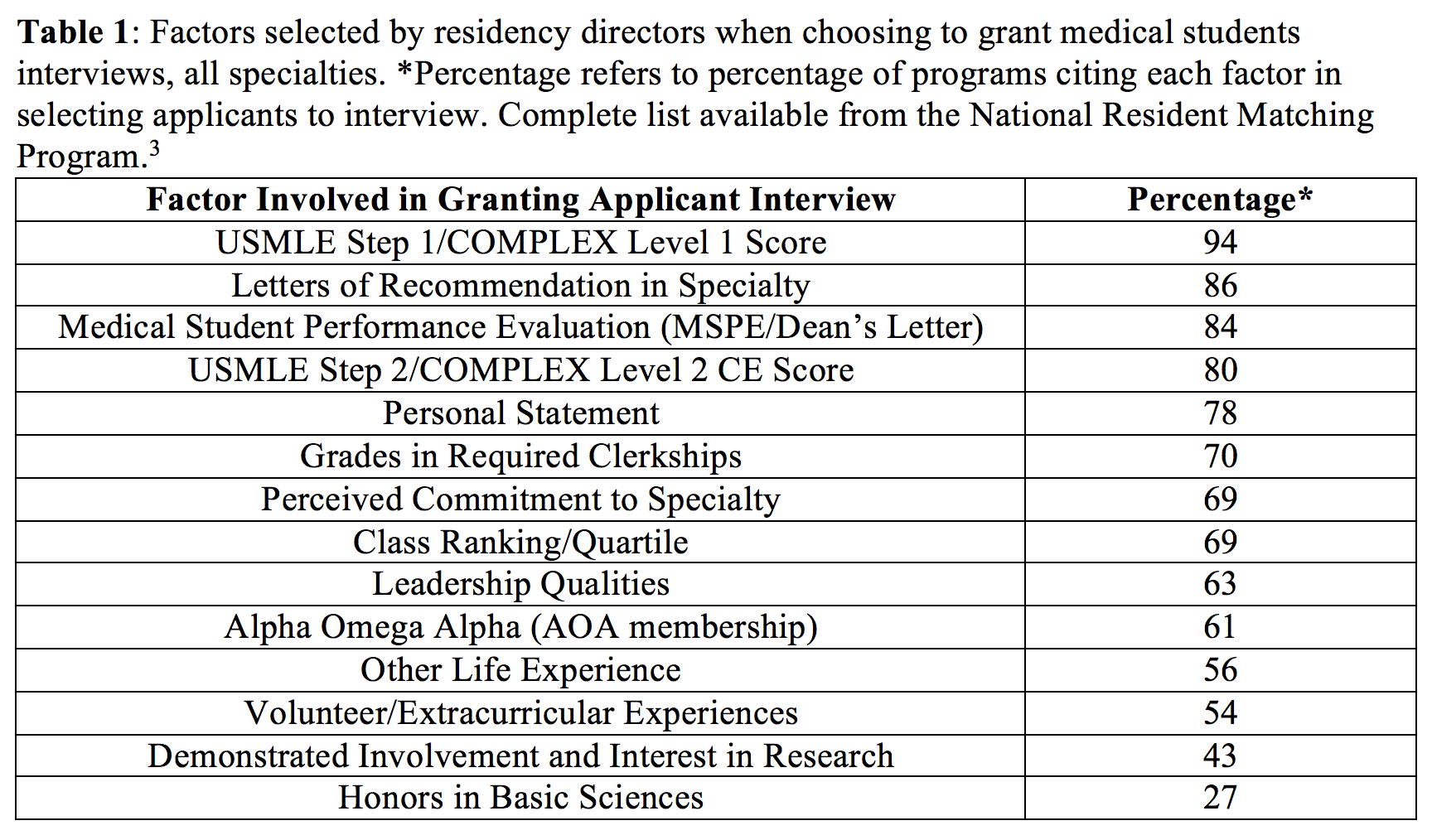
Residency program directors also value a sense of individuality in candidates for their training programs. In 2014, the National Resident Matching Program (NRMP) surveyed over 1,800 residency directors across 22 specialties and Transitional Year programs to evaluate which factors are important in granting applicants interviews. While objective measures such as the USMLE Step 1 and 2 scores topped the list across all specialties, residency directors placed a significant amount of importance on factors highlighting the unique attributes of each medical student, sometimes over objective measures (Table 1)(3). Beyond a threshold of objective measures, medical student success relies on the unique academic, extra-curricular, and life experiences of the individual. It appears, therefore, that there is a dissonance between what medical students may perceive as a successful residency applicant—such as honors in preclinical courses or early involvement in research—and the reality of the successfully-matching medical student. Medical schools should present this data to their students from the very first day of class, reducing the creation of incorrect subjective measures of success that fuel comparisons among peers.
Medical school faculty should also use this data to create opportunities for students to highlight their unique interests. Promoting community volunteerism, research, international pursuits, and interdisciplinary studies, among others, can be achieved by reducing the unnecessary focus on course exam scores. As the NRMP data shows, for instance, 63% of residency directors across all specialties cited leadership qualities to be an important factor in granting interviews as opposed to only 27% of them citing honors in basic sciences courses to be important.
Encouraging learning through application as opposed to high exam scores in the preclinical years will benefit students as they apply for residency programs. Vanderbilt University School of Medicine, for instance, recently implemented a more applications-based education program –Curriculum 2.0—that shortens the standard two-year preclinical curriculum into one while expanding the clinical years to three, opening up time for unique student explorations in the hospital, in the lab, and internationally (4). This can be further optimized by including community activities, research, and involvement in student organizations as factors in ranking students within each class (class ranks are important to many residency directors, as the NRMP data shows), providing a holistic picture of the residency applicant as a scholarly student and a service-minded, passionate human being.
In 2006, Mayo Medical School published the results of its transition from a traditional five-factor, A through F grading system to a pass-fail system, an effort to promote student wellness, professionalism, and learning (5). Their study found that students who were graded on a pass-fail system exhibited less stress, better moods, and even group cohesion with less competition when compared to students in the five-factor grading system. Perhaps of greatest value was that this transition did not affect academic performance or USMLE Step 1 board scores of the students in the new grading system. As the study suggests, creating a hierarchy of any kind in course grades only fosters competition and comparison—and thus negative mental health effects—without any added academic benefit.
In addition to abolishing grading hierarchies, medical schools should work to foster a team-based environment within the classroom as opposed to a competitive one. As everyday hospital observation dictates, the successful treatment of a patient cannot be attributed to a single healthcare professional; rather, it is a group of professionals working constructively and cooperatively that heals the patient. Thus, teamwork in medicine should be integrated into medical education as well. This solution can also be achieved by eliminating grading hierarchies for courses, as the Mayo Medical School study describes, but other documented successful approaches include complementing lectures with medical simulations, problem-based learning sessions, and didactic sessions in team-building (6,7,8).
It is without doubt that many medical students today are consistently stressed due to course rigor and high self-expectations; comparisons among peers will only aggravate that stress, causing students to avoid sharing their true feelings about their transition to medical school and to seek help from classmates. While students can take personal measures to recognize the inevitably negative consequences of interpersonal comparisons, it is the responsibility of all medical schools to put in place practices—such as those I have described above—to help students focus on what really matters: learning the medicine as opposed to acing the exam, and working together as opposed to stressing alone.
After all, in poker the infamous poker face is invaluable to winning the game, for there can only be one winner. But in medical school, we all win the Medical Degree and become physicians.
References
1. Festinger L. A Theory of Social Comparison Processes. Human Relations 1954; 7: 117-140.
2. Liselotte ND, Thomoas MR, and Shanafelt TD. Medical Student Distress: Causes,
Consequences, and Proposed Solutions. Mayo Clinic Proceedings 2005; 80: 1613-1622.
3. National Resident Matching Program. Results of the 2014 NRMP Program Director Survey.
June 2014.
4. Office of Undergraduate Medical Education. MD Curriculum. Vanderbilt University School of Medicine, n.d. Web. 15 Jan. 2016.
5. Rohe DE, Barrier PA, Clark MM, Cook DA, Vickers KS, and Decker PA. The Benefits of
Pass-Fail Grading on Stress, Mood, and Group Cohesion in Medical Students. Mayo Clinic Proceedings 2006; 81: 1443-1448.
6. O’Connell MT and Pascoe JM. Undergraduate Medical Education for the 21st Century:
Leadership and Teamwork. Family Medicine 2004; 36 Suppl: S51-S56.
7. Koh GC, Khoo HE, Wong ML, and Koh D. The effects of problem-based learning during medical school on physician competency: a systematic review. Canadian Medical Association Journal 2008; 178: 34-41.
8. Okuda Y, Bryson EO, DeMaria S Jr, Jacobson L, Quinones J, Shen B, Levine AI. The utility of simulation in medical education: what is the evidence? The Mt. Sinai Journal of Medicine 2009; 76: 330-343.
