Transitioning to medical school is a significant change for most students; this naturally makes it a source of excitement, anxiety, stress, and even fear. Being a successful college student will not necessarily translate to success in graduate/professional school, although many of the same or similar strategies will help. Ultimately, adjusting to medical school is going to depend on the individual student and their school; each curriculum will present unique challenges and each student will handle them in a unique way. Although curricula vary among schools, some concepts are similar across the board. Perhaps the most uniform component of twenty-first century medical school curricula is the fact that they are constantly seeking to improve; thus the adage that “change is life’s only constant” seems to be true, at least of medical schools.
healthcare
The Other Preparations to Make For Clinical Clerkships
The transition to clinical clerkships in medical school comes after two years of lectures, in-class exams, and national board exams. Without a doubt, it is an exciting transition. It is a key stage in the development of a physician, allowing the student to see real patients and to learn from practicing professionals. Clinical rotations requires the student to critically think and to apply the vast amount of information learned in the classroom to new situations. The goal is to learn to come up with a list of differential diagnoses, use the correct confirmatory test, and develop a treatment plan. This is what many students believe will be the bulk of their clinical learning during the third and fourth years. As a result, many students spend most of their time focusing only on the academic preparation for clinical rotations and do not sufficiently prepare themselves to stand out in equally important, but non-academic ways.
20 Questions: Natalie E. Azar, MD – Rheumatology
Dr. Natalie E. Azar is assistant clinical professor of medicine and rheumatology at the Center for Musculoskeletal Care NYU Langone Medical Center, as well as medical contributor to powerwomentv.com, member of the admissions committee for NYU School of Medicine, and instructor of the Physical Diagnosis Course at NYUSoM. She received a bachelor’s degree in psychobiology from Wellesley College (1992), where she was a Phi Beta Kappa (1991), Durant Scholar (1992), and Who’s Who Among American College Students (1991). Azar received her Doctor of Medicine from Cornell University Medical College (1996), with honors for academic excellence in anesthesiology (1998). Dr. Azar completed both an internship and residency in internal medicine at New York University Langone Medical Center (1996-97, 1997-99), and a fellowship in rheumatology at Hospital for Joint Disease, New York University Langone Medical Center (1999-2001).
Hysterectomy or SSRIs?
Reposted from here with permission She was a petite, otherwise well-appearing woman, apprehensively sitting at the edge … Read more
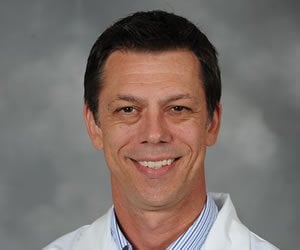
Welcome to Healthcare 5.0: A Conversation with David M. Carlisle, MD, PhD
At this year’s UC Davis Pre-Health Conference, the concept of innovation was on everybody’s minds and lips. There’s no denying that this is an exciting time to be in the medical field; between new technologies, healthcare reforms, and an increasingly global society, things are changing at a rapid pace.
With all this newness and excitement, it’s easy to forget the reason so many of us go into medicine: to help others. And while the topic of his conference keynote was “Healthcare 5.0”, when SDN sat down with David M. Carlisle, MD, PhD, the focus was on caregiving in the most traditional sense.
Q&A with Physician Writer Christine Montross
Dr. Christine Montross is Assistant Professor of Psychiatry and Human Behavior and the Director of Counseling Resources at the Warren Alpert Medical School of Brown University. She works as a staff psychiatrist at Butler Hospital in Providence, Rhode Island. Before attending medical school at Brown, Dr. Montross graduated from the University of Michigan with a Master of Fine Arts in poetry, and undergraduate degrees in French and Natural Resources.
Difficult Interview Questions: Learning To Hit A Curveball Out Of The Park
By Michelle Finkel, MD with CrispyDoc
You put your heart and soul into your compelling, charismatic personal statement; you showcased your accomplishments and drive to succeed in your activities section; and you demonstrated the endorsement of respected faculty allies in your letters of recommendation. Now your hard work has paid off and helped you get a foot in the door: You’ve been invited to interview at your dream medical school or residency program.
Chronicles of a Med Student: Time for a Reality Check
I was about to burst with excitement the minute I started medical school. I’m pretty sure I was actually giddy: like so many other pre-meds, I had dreamt of the day when I would finally put my pretty white coat on and actually start learning about things I cared about (that’s not to say everything I’d learned previously was useless—it absolutely wasn’t, but it wasn’t what I wanted). It felt like the longest road just to get to this point and I couldn’t even begin to fathom what was to come. It really was like the journey had ended…instead of just begun.
Book Excerpt From 11 out of 10: "Prince Albert"
I used to be an Emergency Medical Technician at a very busy Emergency Department. Given that about 70% of all patients that walk in the front door just need little more than a bandage, my job was to treat those low acuity patient under the supervision of a NP/PA or MD/DO. Simple things like removing sutures, bandaging wounds, and assisting the providers in more complicated or invasive procedures. I have three kids that liked to stick stuff where it didn’t belong when they were toddlers and I became quite adept digging things out of ears and noses. Naturally, I became the go-to person for removing foreign bodies and resolving foreign body entrapments in our Emergency Department. I have extracted a ton of weird stuff from ears and noses– things that I didn’t think were possible to get in those spaces to begin with. I had a very high success rate and was generally trusted to be able to handle almost any situation that presented itself.
Getting to Yes: Crafting a Resume for the Medical Field
Since the medical field is full of a wide variety of job opportunities, it is … Read more
20 Questions: Jeffrey M. Whitaker, DPM, FACFAS
Dr. Jeffrey Whitaker knew at a very young age that he wanted to be a doctor, though his specialty remained uncertain until he discovered podiatric medicine as an undergraduate pre-med student. Having graduated Magna Cum Laude with his Bachelor’s degree in Biochemistry from California State University-Long Beach, he later completed a second Bachelor in Cell and Molecular Biology with San Francisco State University, followed by the successful completion of his Doctor of Podiatric Medicine degree from the California College of Podiatric Medicine, which is now Samuel Merritt University. Dr. Whitaker graduated from the DPM program with Honors, ranking 4th in his class, and completed his three-year foot and ankle surgery residency with Western Pennsylvania Hospital, in Pittsburgh.
Blurred Lines: The Doctor-Patient Relationship-in-Training
Reposted from here with permission It is one thing to be a doctor and another to … Read more
Choosing a Specialty: The Generalist vs. the Early-Committer
Many students arrive at medical school with a bias that their liberal arts education has instilled, namely, that they should survey everything before deciding on their specialty. Before medical school, students matriculate at colleges that pride themselves on providing a diverse exposure to a variety of subjects: Computer science majors experience the canon of Great Literature before pursuing a life of code, and English majors can take “Physics for Poets.”
For a generalist student sampling from the buffet of medicine, it can be jarring to sit in lecture next to a classmate who declares on the first day of school that she intends to become an orthopedist. These early-committers appear to have whittled down their choices from day one. They magically become apprentices to a faculty member in their chosen specialty by the first quarter, have a publication by their first year, and seem to possess an intuitive roadmap for applying to residency that the generalist cannot read.
Dental school the second time around: An IDP student perspective
This article is reprinted with permission from the American Student Dental Association. It originally appeared in the Summer 2015 issue of Mouth.
Each year, dental schools across the United States graduate students who were already dentists. Coming from different backgrounds and nations, we are termed IDP, or International Dentist Program, graduates. ID Programs in the U.S. are one of the most incorporating and intensive dental programs around the globe. However, the realization of second graduation involves a different set of struggles that the traditional dental student might not be aware of.
20 Questions : Karen M. Winkfield, MD, PhD, Radiation Oncology
Karen M. Winkfield, MD, PhD, is a radiation oncologist with Massachusetts General Hospital, and she divides her time among clinic research in health equity and hematologic malignancies, teaching as assistant professor of radiation oncology at Harvard Medical School, and a clinical practice treating patients with lymphoma, leukemia, myeloma, myelodysplastic syndrome and other blood cell dyscrasias, and breast and gynecologic malignancies.
Dr. Winkfield received her bachelor’s degree in biochemistry from Binghamton University (1997), and her PhD in pathology (2004) and MD (2005) from Duke University. She completed an internship in internal medicine at Duke and a residency in radiation oncology at Harvard. Dr. Winkfield co-founded and directs the Association of Black Radiation Oncologists, and she’s been published in numerous journals, including the Journal of Biological Chemistry, Journal of the National Medical Association, International Journal of Radiation Oncology – Biology – Physics, Oncology, Journal of the American Academy of Dermatology, and New England Journal of Medicine. She also currently chairs the Health Access and Training Subcommittee for the American Society For Radiation Oncology and is chair-elect of the Health Disparities Committee for the American Society of Clinical Oncology.
How to Make the Most of a Medical School Visit
Once you have been selected for an interview at a medical school, you will have the opportunity to visit the campus. Though your priority during this visit will naturally be to excel in your interview, it is also important that you gather key information from various individuals so that you can make an informed decision when deciding which medical school to ultimately attend. Below are three tips on how to make the most of a medical school visit:
The Risk Involved in Going to Medical School (and How You Can Subvert It)
Most people wouldn’t normally think of medical school as a risky investment. Sure, there are … Read more
The Med-Peds Residency: Big and Small, We Care for Them All
As third year medical students you’re rotating through your general specialties and you think you’re seeing familiar faces but in new places. Isn’t that your newborn nursery resident who assigned APGAR scores, now leading the code in the medical ICU? Some of you may have had similar déjà vu experiences but rest assured, your mind isn’t fooling you. At 79 programs across the USA and Puerto Rico, Combined Internal Medicine and Pediatric residents walk (briskly) through the halls of the hospital carrying both PALS and ACLS cards in our coat pockets. Our minds have been shaped to think broadly and decisively. We carry an air of calmness from our critical care rotations yet we know when to appropriately turn to our goofy side to connect with our patients. Through four years of versatile training, we are training to be the 21st century physician.
The Combined Internal Medicine-Pediatrics (commonly referred to as “Med-Peds”) is a four-year residency-training program that leads to dual board certification in Internal Medicine and Pediatrics. While there are many combined training programs offered in the US, the Med-Peds residency is by far the most ubiquitous and popular program available. During the four years of training, residents undergo a rigorous schedule of rotations ranging from adult and pediatric wards, MICU, PICU, NICU, CCU, Med-Peds clinic and specialty electives. By graduation, residents will have completed a total of 2 years of adult and 2 years of pediatric training. The frequency at which residents switch from one “side” to another changes depending on the individual residency program. The end product is the same: Individuals who are prepared to deal with acute, complex, chronic and preventive care for both adult and pediatric medical conditions. The broad training creates an endless list of career possibilities. We each carve out a niche that best fits the career interest we have in mind.
Fifty Shades of Care: Why Doctors Need to Pay More Attention to their Kinky Patients
Reposted from here with permission. On Valentine’s Day weekend last year I found myself at Paddles, the local … Read more
Five Ways to Make Your Audition Rotation in Anesthesia (or Other Specialty!) a Success
It is that time of year again. Medical school students across the country are preparing applications for residency and pursuing audition rotations at residencies they are hoping to woo into an interview and hopefully to match into their program.
Any audition rotation is a challenge. This is especially true for the anesthesia audition rotation. For medical school students who look great on paper, the audition rotation can either confirm they are a great candidate or confirm the program should not interview/rank them. For medical school students who do not have a stellar record, the audition rotation can open up doors.